Diaper Rash
Diaper dermatitis occurs when the skin’s protective barrier mechanism is compromised. Skin irritants and excessive moisture are common triggers, but it can managed with the ABCDE’s of skincare.
Diaper dermatitis occurs when the skin’s protective barrier mechanism is compromised. Skin irritants and excessive moisture are common triggers, but it can managed with the ABCDE’s of skincare.
Diaper dermatitis occurs when the skin’s protective barrier mechanism is compromised. Skin irritants and excessive moisture are common triggers, but it can managed with the ABCDE’s of skincare.
Diaper dermatitis is a common reason for doctor visits under the age of three. 50 to 65 percent of patients in this age group experience it. This condition affects 25 percent of premature and full-term newborns, and up to 35 percent of babies under one year of age. These rashes are frustrating for parents, and uncomfortable for infants and toddlers. They may be an occasional annoyance, or become a persistent problem. Many types of diaper dermatitis are preventable, but treatment may be necessary for atypical cases.
Most diaper rashes are caused by factors that reduce the skin’s protective barrier mechanism. The outermost layer of the epidermis is the stratum corneum, and its cells have the ability to absorb moisture. In addition, keratin cells release lipids into this layer, creating a waterproof barrier. Skin pH also plays a role. Normal skin is mildly acidic, with a pH ranging from four to six. This acidity promotes the activity of enzymes that protect the integrity of the epidermis and dermis. Mechanical disruption of the stratum corneum, or an increase in pH results in skin that is primed for the development of a rash.
Anything that irritates the skin can promote diaper dermatitis. Friction may occur while cleaning the skin, or from contact with certain diaper materials. Urine, stool, and some skincare products create an alkaline skin pH, and, therefore, limit the activity of protective enzymes. Prolonged and repeated skin contact with irritants leads to dermatitis. The ammonia in urine causes a “burn” type of rash. Diarrheal stools are particularly irritating due to the presence of digestive enzymes. Food allergens can cause skin-irritating diarrhea as well as an atopic rash. However, once the offending food is removed from the diet, the diaper rash improves. In addition, it is easier for bacteria to bind to irritated skin and cause an infection. Staphylococcal aureus and group A streptococcus are the most common pathogens.
Excessive moisture contributes to the development of a diaper rash. Because most commercial diapers are designed to prevent leaks, they create a very warm, humid internal environment. In contrast, cloth diapers are made of organic cotton, so there is no protective barrier against wetness. This moisture, along with an alkaline skin pH, promotes the overgrowth of Candida albicans, a component of normal skin flora. In addition, some infants and toddlers sweat while wearing a diaper, thus creating more trapped moisture.
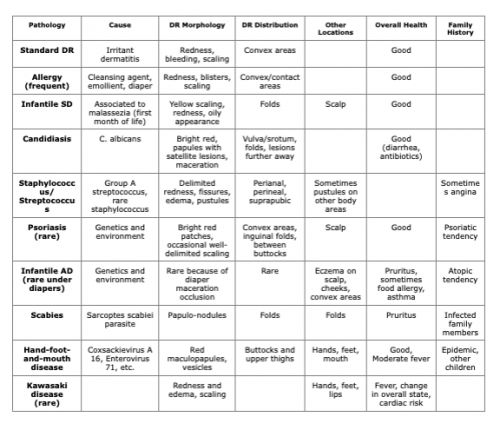
The following graphic details the various types of diaper dermatitis. It may appear on the perineum, buttocks, perianal area, and within intertriginous areas. In boys, scrotal involvement is common in cases of fungal and psoriatic diaper dermatitis.
When soiled diapers are not regularly changed, the risk of diaper dermatitis increases. Aside from a situation of neglect, this phenomenon often occurs when there are multiple caregivers. Each may have a different definition of “regular diaper changes,” and the resulting wet diaper interval is much longer than anticipated. Using cloth diapers exacerbate this problem because wetness stays in contact with the skin for a longer period of time.
Some infants have very sensitive skin, and even “baby-friendly” products cause irritation. Others show skin sensitivity when a new brand of diaper is used. Although baby wipes are both effective and convenient for cleaning urine and stool, some infants react to their ingredients. Candida albicansinfections are a potential side effect of oral antibiotics. These medications reduce the normal bacterial skin flora that prevent fungal overgrowth, resulting in oral thrush and diaper dermatitis.
The American Academy of Pediatrics has developed a mnemonic for their recommendations, the ABCDE of diaper area skincare.
Air: Exposing the skin to air on a frequent basis prevents most diaper rashes.
Removing the diaper for brief periods gives the skin a reprieve from moisture. Once a rash has developed, two to three hours per day of diaper-free time can speed its resolution. Using a hand-held fan before placing a clean diaper can ensure that the skin is as dry as possible.
Barrier: While cleaning, patting instead of rubbing the skin reduces friction. Creams and emollients enhance the lipid barrier function of the stratum corneum. They protect the skin from friction and excessive moisture. Current products contain ingredients such as zinc oxide, petroleum, and lanolin, among others. Baby powders should be used with caution, and those that contain talc are not recommended for infants and children. Talc particles can become aerosolized, inhaled, and then irritate the lungs. Cornstarch powders do promote dryness within the diaper. Candida albicans, however, proliferates in cornstarch, so it should not be used for this type of diaper dermatitis.
Cleaning: Hygiene practices can both prevent and improve diaper dermatitis. Rinsing the perineum under warm water can effectively clean the skin in a non-irritating way. Wet wipes are ideal for cleaning healthy skin. Most are made of cotton, micellar water, and a surfactant, along with pH buffers to help maintain the skin’s acidic pH. There are studies which show more skin protection from the use of wipes than a moist washcloth. Wet wipes with fragrances or potentially harsh ingredients such as sodium laurel sulfate, linalool, and limonene, however, should be avoided. Some infants are also sensitive to wet wipe preservatives, so caution should be exercised for those with atopic skin.
Diapers: Once soiled, diapers should be changed as often as possible. Disposable diapers contain a gel core that absorbs urine and liquid stool, keeping moisture away from the skin. There is a limit to this absorption, however, so diapers should be changed every two hours. Cloth diapers have become increasingly popular, especially in regards to their lower carbon footprint. Many styles are available, including those with attached leakproof but breathable covers. Because these diapers do not have the ability to separate wetness from the skin, they must be changed frequently. Specific laundering techniques are necessary for cloth diapers, and petroleum-based diaper creams can damage the material.
Education: Good hand washing is important, both before and after changing a diaper. This reduces the transmission of bacterial infections, and the need for antibiotics.
A recent study conducted in China, Germany, and the United States supports the ABCDE guidelines. It concluded that the best rash prevention is diligent skin hygiene and topical product use. Frequent diaper changes, including the overnight hours, also reduce the frequency of diaper dermatitis.
Recent studies have evaluated the role of breastmilk in the prevention and treatment of diaper rashes. Breastmilk is naturally fortified with fat-soluble vitamins, calcium, and vitamin B12. These components soften and strengthen skin. Although further research is necessary, positive outcomes have been seen when using breastmilk for diaper rashes.
At times, a diaper rash develops despite the implementation of the ABCDE methods. In these cases, medication may be necessary. Diaper dermatitis caused by Candida albicans overgrowth responds well to topical anti-fungal creams. Versions that are combined with a topical steroid are helpful for cases with significant skin inflammation. Most bacterial infections are treated with topical antibiotic ointments, but oral therapy may be necessary in cases of cellulitis. When scabies is present in the diaper area, there are typically lesions elsewhere. An overnight, head-to-toe skin application of permethrin cream effectively kills the mites. In these situations, fomites should be laundered, and other symptomatic family members should be treated. Psoriatic diaper dermatitis is managed with two week courses of low to mid-potency topical steroid creams. This is often followed by maintenance therapy with topical calcineurin inhibitors. Care must be taken to limit the prolonged use of steroid creams in the genital area to prevent side effects such as skin thinning, local hypertrichosis, and systemic absorption.
https://onlinelibrary.wiley.com/doi/full/10.1111/pde.13495
https://www.karger.com/Article/FullText/501732
https://www.medicaljournals.se/acta/content_files/files/pdf/93/3/3854.pdf
https://pedsinreview.aappublications.org/content/42/1/48
https://www.contemporarypediatrics.com/view/more-stubborn-diaper-rash
https://kidshealth.org/en/parents/diaper-rash.html?ref=search
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7027557/
https://www.medicalnewstoday.com/articles/327289#_noHeaderPrefixedContent
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4228634/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5472239/
